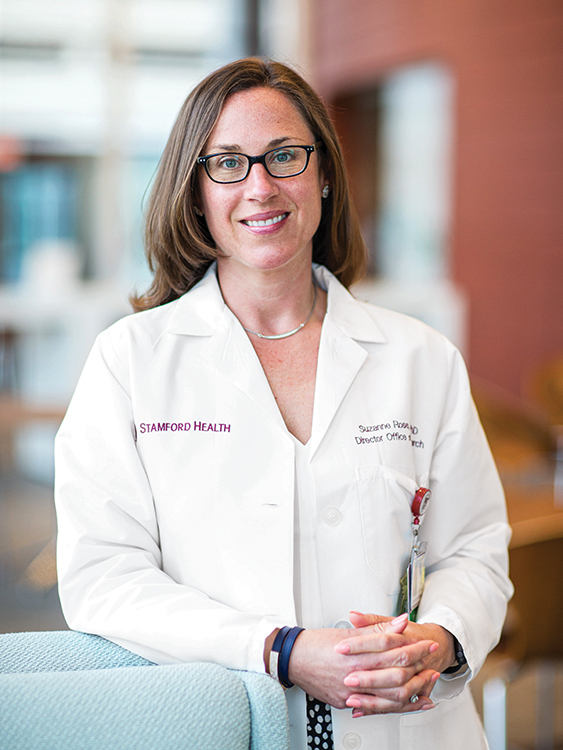
In the early days of the coronavirus pandemic, clinical researcher Suzanne (Simmons) Rose ’99 made a crucial decision that almost certainly saved lives. As patients with the virus flooded ICUs around the country, she spearheaded trials using convalescent plasma that may have tipped the scales between life and death for patients. Before the treatment, initial results show, only 50% of patients survived the virus; afterward, 85% recovered.
“We’ve seen tremendous results in a short amount of time,” says Rose, who is director of the Office of Research at Stamford Hospital. “It gives you hope to say we tried something new and people are living.”
While she loved science from an early age, Rose majored in Spanish at Colgate, attending a study abroad program at the Instituto Internacional in Madrid that was a life-changing experience. “It gave me the confidence to believe in myself and try new things,” she says. After college, she followed her interest in research to a PhD program at Albany Medical College. There, she realized that organizing clinical trials was a perfect fit. “I know how to speak at a scientific level, and I love interacting with patients,” she says.
At Stamford Hospital, Rose helps recruit several hundred patients a year for dozens of trials of experimental drugs to treat heart, kidney, and lung problems; infectious disease; pregnancy complications; and cancer. “We always want to make sure the potential benefits outweigh the risks for our patients,” she says, adding that she is grateful she can offer new treatments that might help patients as well as provide new scientific data. “Some cancer patients don’t have any other options except joining a clinical trial.”
Rose wasn’t able to quickly find a drug trial when COVID-19 began ravaging the hospital in early March. So, she and her colleagues hit upon convalescent plasma as a treatment that had previously worked for diseases including SARS and MERS. When patients recover from a disease, their blood plasma contains antibodies that, when transfused to a new patient, can help fight off the disease. “We said, we have to try something,” Rose says. They scrambled to find donors who had both tested positive and recovered from the coronavirus, in the first week only obtaining four bags of plasma, enough to treat only two patients.
She and her staff continued to push to find plasma donors to treat the more than 40 ICU patients who could potentially benefit from treatment. They were motivated by the fact that some of the patients were Stamford Hospital employees who were now dying. “It was personal to us,” she says. “They weren’t just names; we knew some of these people.” The team made the difficult decision to treat the most severe patients first, even knowing they might not make it. The results they saw were nothing short of miraculous. “We started seeing people who had been at death’s door come off of ventilators,” Rose says. When the first patient they treated — a 70-year-old man who had been on a ventilator for two months — was wheeled out of the hospital, the staff cheered and cried tears of joy.
Eventually Rose was able to secure enough plasma to treat everyone eligible in the three ICUs, and she has since helped to expand the clinical trials to other hospitals in Connecticut, Rhode Island, and Pennsylvania. While she can’t yet say definitively how much the plasma made the difference, she is confident that the data will eventually show the treatment worked. “If we saved even one life, that’s enough for me,” Rose says. “But I think we saved more than that. It made all of the long days and nights completely worth it.”